Authorization Management
We’re on a mission to make
”write-off“ the bad word it should be.
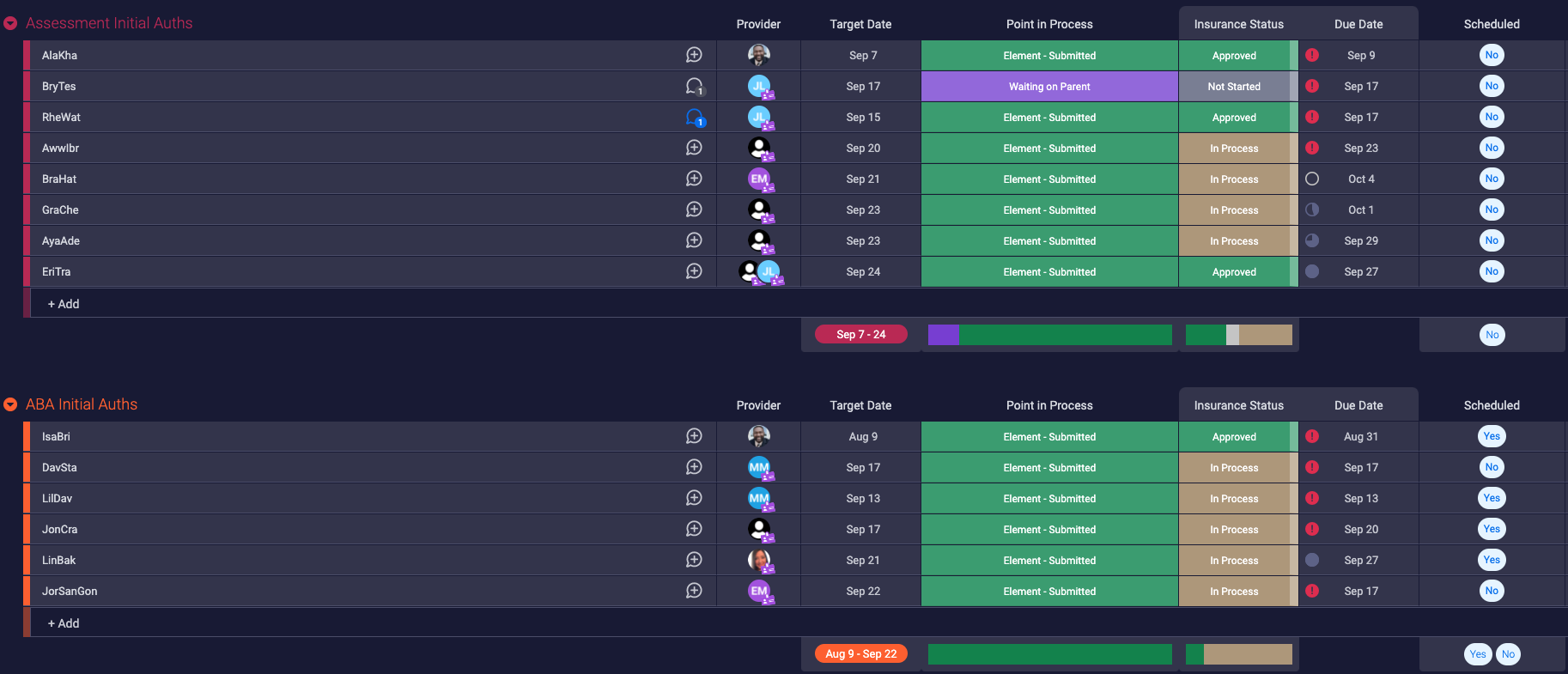
There’s complexity to ABA authorizations. Is auth required for initial assessment (cpt code 97151)? How about direct treatment (97153)? Does it matter if it’s a Medicaid vs. commercial insurance company? If the child has an autism diagnosis or not? Or a different diagnosis? How far in advance do they need to be submitted to ensure coverage? Does insurance back-date these requests?
If you provide critical mental health services (diagnostics, speech language pathology, occupational therapy, counseling, etc.) – particularly in conjunction with ABA – the complexities multiply.
Let us deal with these critical issues that could otherwise drive you crazy. We’ll obtain prior authorization for every service that needs it, every time. So you can stop fretting about your authorizations and focus on the clients you serve.
Putting the ”customer“ back into ”customer portal“
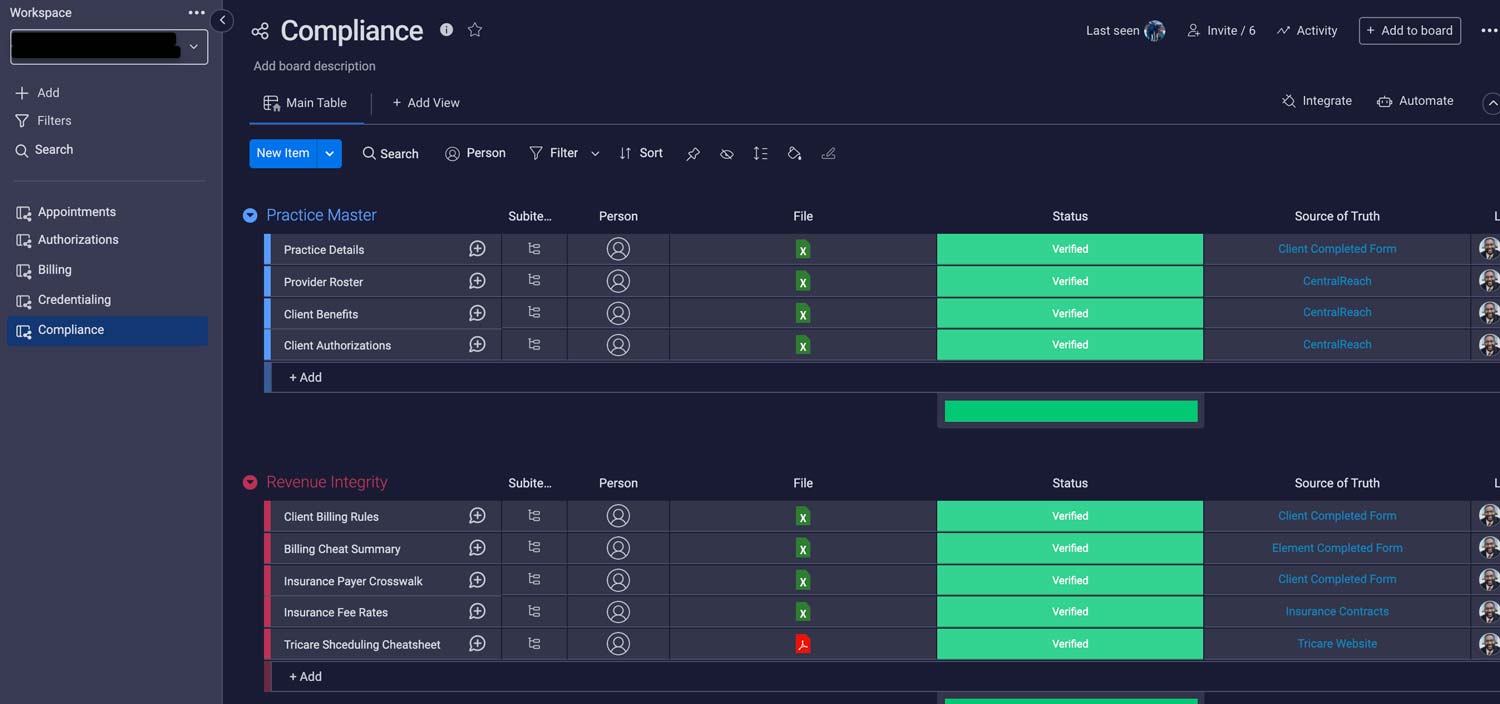
Are you sick and tired of logging into multiple systems that feel like they were designed by Frankenstein? Our easy-to-use customer portal makes it simple for your BCBAs to track authorization deadlines, insurance requirements and much more. Just one more way we’re helping you rest easy at night.
Appeals: we go to bat for you and for your families
These are dreaded words from an insurance rep after you’ve requested 30 hours. It raises so many questions: was this an actual denial? If so, where’s the documentation? Can the decision be appealed? What’s the process? How long will it take? With a client in desperate need of life-changing services, can treatment be provided under continuity-of-care guidelines during the appeals process?
You focus on changing children’s lives. We’ve got this.
Insurance education to empower you
ABA Coding Coalition,
September 2020
